Abstract
Introduction: Primary dural diffuse large B-cell lymphoma (PD-DLBCL) is a rare and aggressive B-cell non-Hodgkin lymphoma that arises in the dura mater, mimicking primary central nervous system lymphoma (PCNSL). While the optimal management is unknown, PD-DLBCL therapy is often mirrored after PCNSL, and aggressive therapy is frequently used. Combining data collected at our institution along with a review of the literature, we provide the most complete analysis of this rare disease entity including data on biology, treatment outcomes, and survival to assist in clinical management.
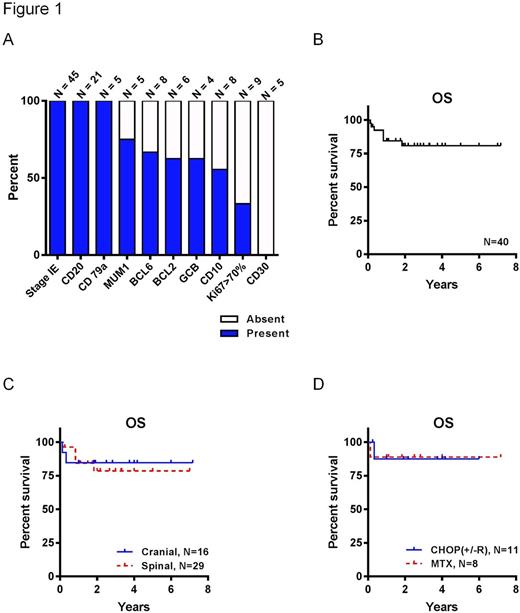
Patients and Methods: A comprehensive review of the literature was conducted on pathologically confirmed intra-cranial and intra-spinal cases of PD-DLBCL reported from Jan 1st 1992 to July 1st 2017 in PubMed. Key words used (single or in combination) included: primary dural lymphoma, PDL, diffuse large B-cell lymphoma, DLBCL, and primary diffuse large B-cell lymphoma dura mater. Data were tabulated regarding the following 16 variables: tumor location (cranial vs. spinal), age, gender, disease stage, cell of origin (germinal center B-cell like (GCB)-DLBCL vs. activated B-cell like (ABC)-DLBCL), CD20, CD10, CD79a, CD30, BCL2, BCL6, MUM1, Ki-67 (above or below 70%), type of chemotherapy, use of radiation therapy, and overall survival (OS). Data were reported as percent and total number of cases with available information of each variable.
Results and Discussion: Out of 235 screened cases, 47 cases of PD-DLBCL were detected from 26 distinct sources. Two cases were excluded for unclear definition about site of origin (dural vs. subdural). In total 45 cases were included in our analysis. Sixteen of these cases were intra-cranial and 29 were intra-spinal. Median age was 59 years at the time of diagnosis. Incidence was nearly equal between women (22/45) and men. When tested, CD20 was positive in each instance (21/21). Using Hans criteria when possible to determine cell of origin, 3 cases were classified as ABC-DLBCL and 5 as GCB-DLBCL, confirming the representation of both subtypes in PD-DLBCL. Ki-67 fraction was given in 9 cases, 6 of which were less than 70%, reflecting an overall less aggressive tumor behavior. The remainder of studied markers are detailed in Figure 1A. Interestingly, all cases were stage IE. Survival data available from 40 cases showed an OS of 84% at 1 year, and 81% at 5 years (Figure 1B), which compares favorably to PCNSL and matches early-stage DLBCL. Tumor location (intra-cranial vs. intra-spinal) did not impact OS (P=0.82; Figure 1C). Significant heterogeneity existed in regards to treatment choices. Initial chemotherapy regimen was reported in 19 cases with available survival data. Eleven patients received a combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP), 6 of which additionally received rituximab (CHOP-R). Eight patients received high-dose methotrexate (MTX) based therapy. Interestingly, no difference in OS was observed between CHOP vs. MTX-based therapy (P=0.97; Figure 1D), suggesting that PD-DLBCL should be treated as DLBCL rather than PCNSL. Moreover, all patients who received rituximab in addition to CHOP remained disease free and alive. Radiation therapy was given often (25/29) in treatment of spinal disease, but rarely (4/16) when treating cranial disease. Three patients received whole brain radiation therapy, twice following CHOP and once following MTX. The use of radiation therapy did not impact OS (data not shown).
Conclusion: PD-DLBCL is an exceedingly rare subtype of DLBCL, GCB- or ABC-derived, and equally seen in both genders. The good outcomes seen with CHOP-R suggest that these cases should be treated like DLBCL rather than PCNSL, obviating the need for the more toxic high-dose MTX-based regimens or radiation therapy. The durable responses following CHOP-R also confirm that PD-DLBCL is not protected by the blood brain barrier.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal